Health insurers can play a critical role in making ALS livable for everyone, everywhere, but all too often barriers are erected that prevent people from accessing the health care services they need.
One of the more common ways public and private insurers make it difficult to access essential health care is through the use of prior authorizations, a process used by health insurers to control costs. While many insurers use prior authorization to some extent, Medicare Advantage plans have been criticized for using it excessively to the detriment of people living with ALS.
Prior authorization requests must be submitted by the health care provider who must document why a particular medicine, treatment or piece of medical equipment is needed. Providers are often frustrated because submitting prior authorization requests is time consuming – especially when it must be done for every patient. And while the provider has direct contact with the patient, the person making the decision for the insurance company may have very limited experience or make the decision based on the “average patient.”
In addition, an insurance company may require a patient try a medication or use a piece of equipment that is less effective and “fail first” before granting approval for the care the physician has prescribed. When care is denied, there are multiple layers of internal and external appeals that can be made – each is time consuming and has their own challenges.
According to a recent ALS Focus survey, approximately one in three participants report having care prescribed by their physician delayed or denied as the result of prior authorization requests. These denials were most often for medications, mobility equipment with necessary accessories, or in-home care services.
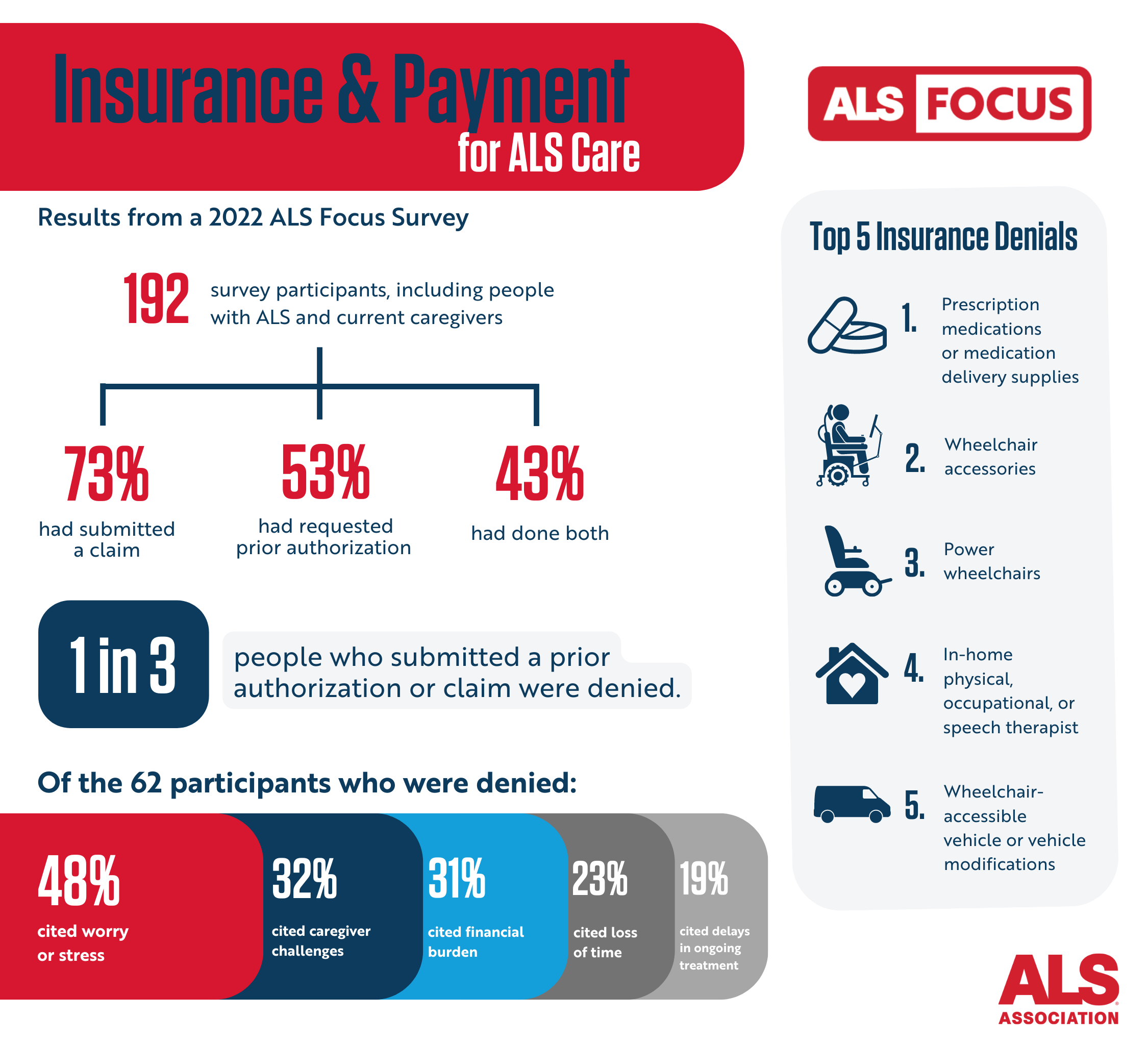
The burden of making an appeal often falls primarily on the patient and their family. While the provider must continue to submit medical information, the person living with ALS must take on fighting the insurer to secure the care the provider has prescribed. In the Focus survey, people living with ALS indicated they often did not try to appeal.
Participants that did appeal noted they often had to appeal up to three times and wait up to six months for a final resolution. Following the appeal process, roughly a third of prior authorizations and claims were still denied or only partially granted, resulting in some people living with ALS having to pay out of pocket or not receive the care or service they needed.
The results of this survey also demonstrate the high burden that denials of essential ALS care place on people living with ALS. Many participants noted that jumping through the hoops of these processes, even if it eventually results in an approval, puts additional strain on individuals and families already dealing with so much.
We are committed to ensuring our community is receiving the timely care they need without the hassle. Earlier this year we filed a formal objection to health insurer CIGNA for the company’s decision to exclude Relyvrio from its formulary as part of the continued fight for access to approved treatments. We shared the letter with the Centers for Medicare and Medicaid Services, the Veterans Administration and state insurance commissioners.
UPDATE – APRIL 2024: Relyvrio was voluntarily withdrawn from the market by Amylyx following a phase 3 trial that failed to show it was effective. The ALS Association stands by its decision to push for early approval of Relyvrio given the promising phase 2 trial data and the safety of the treatment. At the time, we said that if it turns out to be ineffective, at worst, people living with ALS would have taken an ineffective therapy without risk of harm. If it was indeed effective, delaying access would have meant that people living with ALS would have lost two years of being able to take a life-extending therapy. In the interests of transparency and education, we are leaving this information up for future reference. People living with ALS need life-saving treatments and we are working as urgently as possible to advance the many more potential treatments in clinical trials.
Barriers to access are extended to durable medical equipment as well.
One in four respondents to another recent ALS Focus survey said they had to pay out of pocket for the cost of their power wheelchair, with 47 percent saying their insurance company refused to pay for their power wheelchair seat elevation. Moreover, fifty percent of respondents said they had to pay out of pocket for their portable ramp or rollator as well.

Recently, the ALS community scored a big win when Medicare added power seat elevation systems in power wheelchairs as a benefit for disabled individuals including people living with ALS, deeming the technology medically necessary.
Unfortunately, we also know people with ALS are increasingly being denied noninvasive ventilators by Medicare Advantage plans. It is a heart-wrenching reality adding another layer of torment to an already devastating journey.
This is often done through a process known as step-therapy, or fail-first, a process that requires patients to try one or more medications specified by the insurance company, typically a generic or lower cost medicine. Patients must then fail on the medication before allowing a “step up” to another medicine that may be more expensive for the insurer.
In the case of noninvasive ventilators, this could mean insurers force someone living with ALS to try a lower-cost ventilation machine and prove that it is not working before gaining access the equipment they truly need.
It is critically important insurers understand noninvasive ventilators are not a luxury, but a lifeline for ALS people.

Physicians caring for people with ALS are in the best position to determine the course of care and the type of respirator needed, not insurers’ authorization and utilization staff. People living with ALS deserve the full benefit of their doctor’s experience and expertise, especially where it is focused on supporting their ability to breathe.
We recently joined the American College of Chest Physicians (CHEST) to challenge United Healthcare’s practice of delaying and denying medically necessary noninvasive ventilators for patients living with ALS, while also notifying insurance regulators about the practice.
Throughout this month we will be shining a spotlight on some of the ways insurance companies restrict access to essential health care needs and ways the ALS community can fight for better coverage policies that make ALS livable while we continue the search for a cure.
To learn more about Medicare and better understand insurance and benefits for people living with ALS, visit our website HERE.
To continue to follow stories about people living with ALS in the community and learn more about the disease, subscribe to receive our weekly blogs in your inbox HERE or follow us at als.org/blog.


Join the conversation. Please comment below.