Dr. Aaron Gitler and his colleagues recently published a paper in the August 12th issue of Science uncovering a potential new therapeutic target aimed at C9orf72 ALS, supported by The ALS Association. He found that inhibiting just one protein, called Spt4, significantly reduced toxicity caused by the C9orf72 repeat expansion. Learn more about how he used a simple model, yeast, to make this discovery and its therapeutic potential to treat ALS. And join us on November 7th to hear from Dr. Gitler during The ALS Association research webinar series (see details below).
What is your academic background?
I am from Philadelphia and went to college at Penn State and then University of Pennsylvania for graduate school, where I studied Developmental Biology for my Ph.D. I completed my postdoc fellowship at the Whitehead Institute at the Massachusetts Institute of Technology (MIT) under the mentorship of Dr. Susan Lindquist. There I studied protein misfolding and aggregation and learned to use yeast genetics to study how the protein alpha-synuclein, which is involved in Parkinson’s disease (PD), could impact cellular pathways. I moved back in 2007 to U. Penn to start my own laboratory in the Department of Cell and Developmental Biology. In 2012, I moved to Stanford University in California in the Department of Genetics, where I currently run a research laboratory.
How did you get involved in ALS research?
My career in ALS research started during my postdoc when I studied yeast to better understand alpha-synuclein and to perform screens for Parkinson’s disease modifiers. I started thinking about starting my own lab at the end of 2006 when a big breakthrough in ALS happened – the discovery of TDP-43, an RNA-binding protein that aggregates (forms clumps of protein) in neurons of virtually all people living with ALS. This was almost 10 years ago.
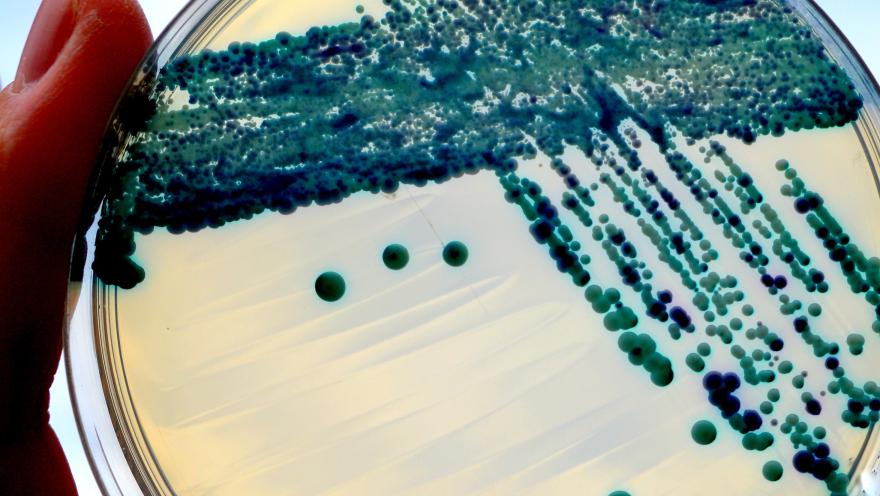
I started with TDP-43 and asked, “What happens if I expressed TDP-43 in yeast?” It formed cytoplasmic puncta and was toxic in yeast. This seemed like a great launching pad to start studying more about TDP-43. It was great timing!
One of the first experiments we performed was a genetic screen to try and find yeast genes that could counteract TDP-43’s toxic effects. One of the strongest hits from that screen was the yeast gene PBP1. In later experiments, we found that the human version of this gene, which is called Ataxin 2, is a risk factor for ALS in people. In a way, this validated the approach of using a simple model system like yeast, showing that it has direct relevance to humans. My lab continues to work on ALS. We have several projects now focused on the C9orf72 gene and are learning more about how Ataxin 2 contributes to ALS.
Has the ALS Ice Bucket Challenge impacted your research?
Not directly, but it has been transformative for the ALS field and has made a major impact. It helped many labs in the field and other labs started studying ALS that may not have in the past. It is a phenomenal success to get people thinking of ALS.
Please explain the ALS Spt4 project that was recently published as a collaborative effort.
The most common genetic cause of ALS is a mutation in a gene called C9orf72. In this gene, there is a stretch of DNA in which six letters are repeated several times - GGGGCC. Normally this is repeated two to five times in a row, but it can get expanded to several 100 or several 1000 times. This massive expansion of the six-letter repeat causes a large portion of ALS.
How does this mutation cause ALS? Many researchers are trying to figure this out. The mutation is present in a non-coded region of the gene, meaning that it is present in the part of the gene that does not make protein. But having this huge repeat placed in the middle of the gene could cause a decrease in the ability for that gene to be expressed, leading to loss of function of C9orf72. We also know that the DNA repeat is transcribed (made into messenger RNA (mRNA)) and the RNAs build up inside of the nucleus of patients that have this mutation. The RNAs can accrue into RNA clumps that could cause other RNAs to be sequestered within these clumps leading to RNA toxicity. Thirdly, that repeat could be produced into protein, in an ATG-independent (alternative) manner of protein translation (converts mRNA into protein). Those proteins that are produced are built up in people that have the disease.
So there are three different pathways of C9orf72 disease that researchers are trying to understand. Even if we do not know if it is RNA or protein causing toxicity, there may be a simpler therapeutic strategy. We could stop production at the higher level of RNA or protein, so we do not have to determine if it is RNA or protein that is toxic. We could simply shut down expression of the gene before it is made into RNA or protein.
There has been a lot of effort to develop a therapeutic strategy called antisense oligonucleotides (ASOs), which are short stretches of a modified form of DNA that are stable and can precisely recognize RNA of interest and bind to it, leading to its destruction. It finds the RNA of interest and targets it for degradation. It works well and can get rid of the C9orf72 repeat expansion in model systems.
Recently, researchers found that not only the RNA repeat is expressed and accumulates, but also the antisense version (in the reverse direction) is also transcribed. The GGGGCC will now be GGCCCC and those also accumulate in distinct foci. We know that if you have a great drug that targets GGGGCC, you are still left with the antisense transcript and vice versa. Researchers can make a new type of ASO to also target this antisense strand, which researchers are doing, but it can be a challenge.
In our paper, we figured out a way to, in one fell swoop, get rid of both the sense and antisense transcripts. This was based on work by others who identified a yeast transcription factor, called Spt4.
Spt4 is an interesting molecule that is selectively required for transcription of long trinucleotide (CAG) repeats (another type of repeat expansion). Think of RNA polymerase as a machine that is going along the DNA and transcribing it into RNA. When it encounters a long stretch of CAGs, it has trouble transcribing and staying on the DNA to do its job. Spt4 acts like an accessory factor to help clamp on the RNA polymerase to the DNA and keeps it going through these long CAG repeat stretches. If you eliminate Spt4, the polymerase cannot transcribe DNA into RNA anymore. Its elimination does not affect other normal gene expression. It only targets genes with long trinucleotide repeat expansions.
We read that paper and thought, “Could Spt4 be involved in the transcription of long hexanucleotide repeats similar to what we observe in C9orf72 repeat expansions?” We tested it in yeast and sure enough, both the sense and antisense transcripts were reduced when we deleted Spt4. We then tested this in C. elegans (microscopic worms) and fruit fly models. Importantly, we tested in this in-patient skin cells, called fibroblasts that have the C9orf72 repeat expansion, and in all models, we observed the same results.
Read the paper here:
Spt4 selectively regulates the expression of C9orf72 sense and antisense mutant transcripts.
Kramer NJ, Carlomagno Y, Zhang YJ, Almeida S, Cook CN, Gendron TF, Prudencio M, Van Blitterswijk M, Belzil V, Couthouis J, Paul JW 3rd, Goodman LD, Daughrity L, Chew J, Garrett A, Pregent L, Jansen-West K, Tabassian LJ, Rademakers R, Boylan K, Graff-Radford NR, Josephs KA, Parisi JE, Knopman DS, Petersen RC, Boeve BF, Deng N, Feng Y, Cheng TH, Dickson DW, Cohen SN, Bonini NM, Link CD, Gao FB, Petrucelli L, Gitler AD. Science. 2016 Aug 12;353(6300):708-12.
What are your next steps?
We are trying to find small inhibitors of Spt4. We would love to have a small molecule that inhibits the function of Spt4 and then we could start testing the inhibitor’s safety and efficacy.
How do you compare your method with antisense oligonucleotide technology?
It is a different approach. We showed the proof of concept – target Spt4 and get rid of both sense and antisense C9orf72 transcripts. I want to emphasize that once we find inhibitors of Spt4, we have to optimize the chemistry of the potential compound and evaluate the safety and efficacy of the strategy, along with dosing. Right now there is not a compound ready for this approach to use as a therapy to treat ALS.
What’s the impact of your project on the ALS field?
We were able to decrease both C9orf72 sense and antisense transcripts just by simply targeting one protein, Spt4. This work was started in yeast and then validated in worm, flies, and in-patient cells – all harboring the C9orf72 mutation. Inhibiting Spt4 serves as a potential target for ALS therapy.
What makes yeast so powerful?
Even though these are complicated human diseases, we hypothesize that at their core are defects in basic cell biology. If that is true, we then should be able to use very simple models to explore all major pathways, which are conserved and functional.
Importantly, we are not studying or modeling the disease in yeast. ALS is a complicated disease involving interactions between multiple cells and tissue types. What we are studying are the molecular and cellular interactions of proteins and pathways in the cell, which we believe are very relevant to the disease.
There are many advantages to yeast biology. Yeast cells divide and grow very rapidly. When disease proteins aggregate in the brains of patients, it takes decades. In mice, it takes a year or two. In yeast, we can express an ALS protein, like TDP-43 for example, and in one hour, we see aggregation. We can also do comprehensive genome-wide screens that are rapid and robust. My small laboratory of students and postdocs can do these experiments very rapidly and the techniques are not complicated. Because the experiments are relatively inexpensive, with donor money, we can get a lot of information in a short amount of time.
What are you the most excited about when it comes to ALS research?
Right now it is such an exciting time in ALS research! In genetics, we now know the genetic causes of a large number of ALS cases. We have all these new targets, pathways, and hypotheses that in the coming years we can aggressively work on to test. It is a very great time to be in ALS research!
Equally exciting, there have been some really encouraging advances in therapeutic strategies, especially involving antisense oligonucleotides (ASOs). There have been huge advances with this in Spinal Muscular Atrophy (SMA) in a clinical trial by Ionis Pharmaceuticals and Biogen. Now ASO clinical trials in ALS for SOD1 mutation carriers are ongoing and there are plans for C9orf72 ASO trials in the years to come. Now that we are learning the molecular players, we can start coming up with additional therapeutic strategies.
I really mean it that it is an exciting time in ALS research. My lab is very excited and working harder than ever!
Who are your collaborators on this project?
This is a joint collaboration with my laboratory and Dr. Leonard Petrucelli’s laboratory (Mayo Clinic, Jacksonville, Fla.). Our lab worked with yeast and some human cells, Dr. Petrucelli worked with the worms and some human cells and Dr. Bonini (University of Pennsylvania, Philadelphia, Pa.) worked on the fly model. Dr. Fen-Biao Gao’s laboratory (University of Massachusetts Medical School, Worcester, Mass.) worked on human neurons. It was a team effort. This is a great example showing that you can start with a simple model like yeast and validate your findings in other organisms like worms, flies, and human cells. First authors, Drs. Nicholas Kramer, Yari Carlomagno, and Yong-Jie Zhang all contributed equally to this paper.
Is there something you would like to share with people living with ALS about your lab?
We are really working with intense focus and purpose trying to come up with new ideas and approaches to help people with ALS and to come up with therapeutics for ALS. That really drives us. We are inspired when we meet individuals living with ALS at meetings. We always thinking about them in our research.
Learn more about this exciting project! Read the related press release and blog post.
Join us for Dr. Gitler’s upcoming webinar on November 7th.
Title: Expanding mechanisms and therapeutic targets for ALS
Date: Monday, November 7, 2016
Time: 4:00 p.m. EST

Join the conversation. Please comment below.